




Is Hospice the answer?

Angels Care Hospice, part of the AngMar Medical Holdings, Inc. network, is a premier provider of hospice services in the communities we serve. Our comprehensive, holistic approach to hospice care centers around reducing the fear and burden associated with the end of life journey. This approach allows our patients and their families to live the fullest and most meaningful life possible wherever the patient calls home, including assisted living facilities, hospitals or long-term care facilities.
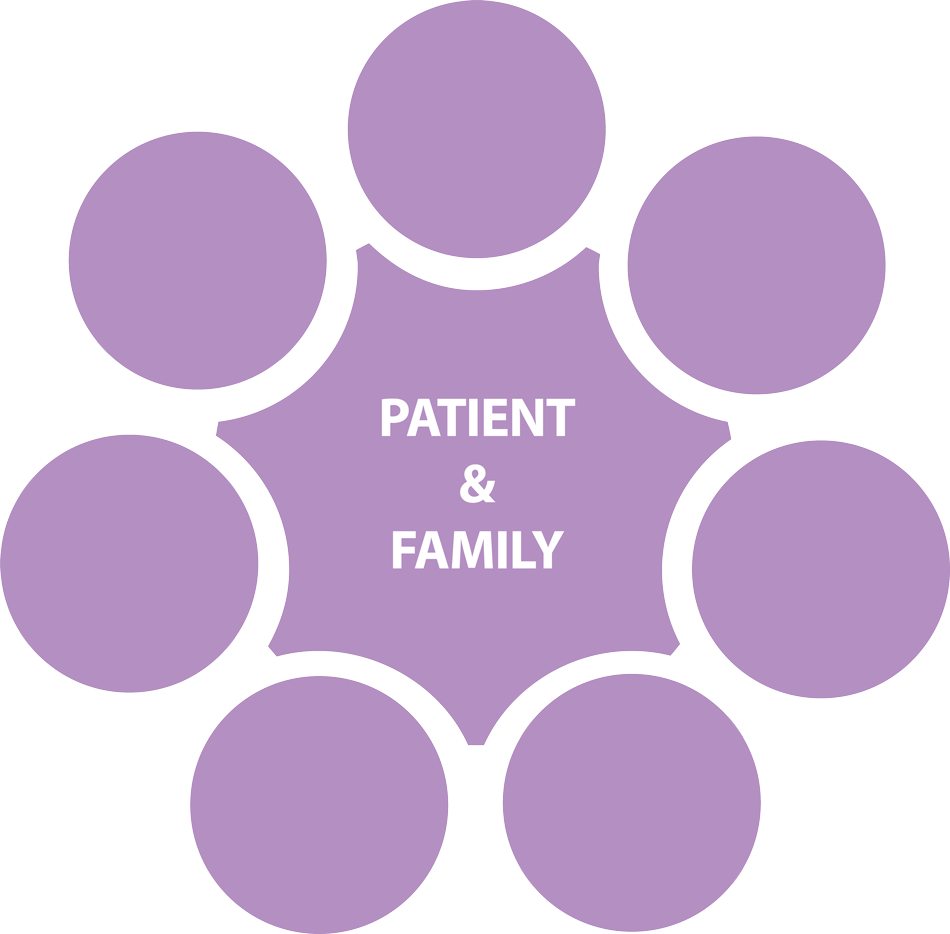
Doctors
(Angels Care Hospice Medical Director and Patient’s Attending Physician) Oversees the patient’s plan of care and the Interdisciplinary Team.
Nurses
Makes regular patient visits, provide case management and provides education to help the caregiver(s) understand the best way to care for their loved one.
Social Worker
Assists the patient and caregiver(s) with advanced directives, helps with legal and financial concerns and identifies community resources, when needed.
Hospice
Aides
Assists the patient with activities of daily living (ADL), if needed, such as bathing, dressing and eating.
Chaplain
Provides non-denominational spiritual support, while respecting the faith and beliefs of the patient.
Bereavement
Counselor
Assesses the bereavement risk for the caregiver(s). Provides support to the patient’s caregiver(s) for at least 13 months after the patient passes away.
Volunteers
Are trained in hospice care and can visit with the patient and provide relief for the caregiver(s).
Our Interdisciplinary TeaM
Hospice & Palliative
Care Basics
Find An Office
Is this not the location you need? Search Angels Care Hospice network of multiple agencies with locations in five states, including Arizona, Kansas, Nebraska, Oklahoma, Texas.
When is it time for Hospice?
When a patient has a terminal illness and is certified by a physician as having a life expectancy of six months or less, they are eligible for hospice care. The patient must also want to choose comfort measures over aggressive treatment. Hospice is proven to be the most effective the earlier a patient starts receiving care and the number one complaint from families is they wish they had known about hospice sooner.
Paying for Hospice
If a patient is medically eligible for hospice care, hospice services are 100% covered by Medicare and Medicaid. Medications, equipment and supplies that are related to the hospice diagnosis and prognosis are covered. Private insurance plans may also provide hospice coverage. We will contact your insurance to verify hospice coverage.

